Summary: The expense of vasectomy reversals is an important factor that discourages couples wanting to have another child. One Stop Medical Center has been offering $2950 all inclusive for an affordable vasectomy reversal service, helping couples conceive children naturally.
 MINNEAPOLIS, MN (March 12th, 2022) – There are approximately half a million men who undergo a vasectomy every year in the U.S. About 7% of them would want a vasectomy reversal. Whereas the cost of vasectomies is usually less than $1000 and are covered by most insurance companies, reversals are not, so couples have to pay for the expensive procedure with cash. If the reversal is performed in a hospital or surgical center, this, in turn, accelerates the cost, further discouraging couples wanting to have another child.
MINNEAPOLIS, MN (March 12th, 2022) – There are approximately half a million men who undergo a vasectomy every year in the U.S. About 7% of them would want a vasectomy reversal. Whereas the cost of vasectomies is usually less than $1000 and are covered by most insurance companies, reversals are not, so couples have to pay for the expensive procedure with cash. If the reversal is performed in a hospital or surgical center, this, in turn, accelerates the cost, further discouraging couples wanting to have another child.
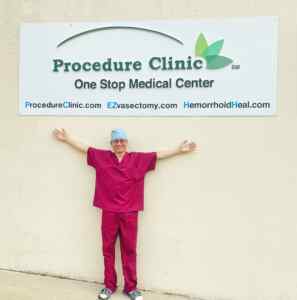
One Stop Medical Center has been offering an Affordable Vasectomy Reversal Service in the past nine years. It continues to Offer $2950 all inclusive for a vasovasostomy procedure.
The aim of vasovasostomy is to reconnect the vas where it was severed at the time of vasectomy, making it a true reverse vasectomy, which makes the most sense for men whose intervals are short (less than 10 years vasectomy) . Vasovasostomy (VV) takes about two hours. It is performed under local anesthesia, similar to the anesthesia used for vasectomy but with a longer-acting drug. Continuity of both vas tubes can be restored with micro-surgical techniques through a single small incision with the assistance of magnification.
We are able to lower your costs by not charging any facility fees and anesthesia fees, but never sacrifice our quality of service. The medical director, Dr. Steven Shu, is an expert in office procedures who is dedicated to helping couples conceive children naturally, and he performs almost 200 vasectomy reversal procedures every year.

 The fear of increasing one’s risk of prostate cancer has stopped some men from undergoing a
The fear of increasing one’s risk of prostate cancer has stopped some men from undergoing a  If you’re looking for a natural, inexpensive way of boosting sperm quality and overall fertility, the answer may lie within…tomatoes?
If you’re looking for a natural, inexpensive way of boosting sperm quality and overall fertility, the answer may lie within…tomatoes? From self-order kiosks to robot vacuum cleaners and robot cafes, the rise of robot-assisted experiences in recent years has been undeniable. But would you ever consider participating in a robot-assisted surgical procedure?
From self-order kiosks to robot vacuum cleaners and robot cafes, the rise of robot-assisted experiences in recent years has been undeniable. But would you ever consider participating in a robot-assisted surgical procedure? However, costs aside, it’s still noteworthy to highlight the reliability and effectiveness of robot-assisted vasectomy reversals.
However, costs aside, it’s still noteworthy to highlight the reliability and effectiveness of robot-assisted vasectomy reversals.  1. Walnuts
1. Walnuts 5. Dark Chocolate
5. Dark Chocolate In a landmark study from the Vasovasostomy Study Group (VVSG) published in 1991, Dr. Arnold Belker and four other expert microsurgeons examined various facets of vasectomy reversal, including the risk of birth defects. Their trial, which followed 291 children born post-vasectomy reversal, found that only three of the 291 subjects displayed birth defects. That’s a one percent birth defect rate.
In a landmark study from the Vasovasostomy Study Group (VVSG) published in 1991, Dr. Arnold Belker and four other expert microsurgeons examined various facets of vasectomy reversal, including the risk of birth defects. Their trial, which followed 291 children born post-vasectomy reversal, found that only three of the 291 subjects displayed birth defects. That’s a one percent birth defect rate.  You may be familiar with the term “antibodies” as “something that helps the body ward off disease,” but the notion of sperm antibodies might seem counterintuitive. After all, why would the body want to destroy perfectly good sperm?
You may be familiar with the term “antibodies” as “something that helps the body ward off disease,” but the notion of sperm antibodies might seem counterintuitive. After all, why would the body want to destroy perfectly good sperm? After undergoing a vasectomy reversal, patients can expect a recovery process similar to that of their original vasectomy. Pain and swelling in the groin is to be expected for about 1-3 weeks, but most patients are able to return to work and daily activities within one week. Below is a breakdown of what to expect for post-surgery care and recovery:
After undergoing a vasectomy reversal, patients can expect a recovery process similar to that of their original vasectomy. Pain and swelling in the groin is to be expected for about 1-3 weeks, but most patients are able to return to work and daily activities within one week. Below is a breakdown of what to expect for post-surgery care and recovery:
 Myth: In Vitro Fertilization (IVF) is quicker and easier than having a vasectomy reversal.
Myth: In Vitro Fertilization (IVF) is quicker and easier than having a vasectomy reversal. Myth: Couples should not try to conceive right after a vasectomy reversal for fear of a “leftover, defective sperm.”
Myth: Couples should not try to conceive right after a vasectomy reversal for fear of a “leftover, defective sperm.”