Introduction
Vasectomy is a widely chosen and highly effective form of contraception among men. However, life circumstances can change, prompting some men to reconsider their decision and pursue parenthood after undergoing a vasectomy. In such cases, vasectomy reversal emerges as a viable option to restore fertility. Although vasectomy reversal is generally successful, it’s crucial to be aware of potential factors that can influence the procedure’s outcomes. This blog explores the impact of anti-sperm antibodies in patients who have undergone vasectomy reversal.
 Anti-sperm Antibodies: What Are They?
Anti-sperm Antibodies: What Are They?
Antibodies are blood proteins produced by the body’s immune system in response to specific antigens, which can include elements like bacteria, viruses, cancer cells, and foreign substances in the bloodstream. These antibodies play a critical role in targeting and neutralizing potential threats to the body. However, in some cases, antibodies can act against the body’s own cells, as observed in various autoimmune diseases.
Anti-sperm antibodies, specifically, are proteins generated by the immune system that target and attack sperm cells. Under normal circumstances, the immune system recognizes sperm as part of the body, and thus, does not initiate an immune response against them. However, when sperm comes into contact with the bloodstream, as can happen following a vasectomy, the immune system may treat it as an invasive foreign entity, leading to the development of anti-sperm antibodies.
It’s important to note that, in usual circumstances, sperm remains largely segregated from the bloodstream due to the presence of the blood-testis barrier. This barrier prevents direct contact between sperm and blood, maintaining sperm’s status as non-threatening to the immune system. However, disruptions to this barrier, such as through trauma, surgery, infection, cancer, or congenital defects, can expose sperm to the bloodstream, potentially triggering immune responses and the development of anti-sperm antibodies.
Effects of Anti-sperm Antibodies in Vasectomy Reversal Patients
Studies have revealed that anti-sperm antibodies are present in varying percentages of men in different populations: approximately 8% to 21% of men in the general population, 9% to 36% of infertile patients, and 70-100% of men following a vasectomy. It’s important to clarify that undergoing a vasectomy does not typically lead to the development of autoantibodies in men, except in the case of anti-sperm antibodies. There is also no substantial evidence linking the development of anti-sperm antibodies after vasectomy to immunological or other diseases.
The Relationship of Anti-sperm Antibodies with Vasectomy Reversal Procedures
The impact of anti-sperm antibodies on fertility following vasectomy reversal is not entirely clear. While it is true that 79% of men tested after a vasectomy exhibit elevated anti-sperm antibodies, these levels are not typically significant enough to cause a substantial decrease in fertility. In most men, these antibodies do not result in significant, long-term side effects arising from vasectomy.
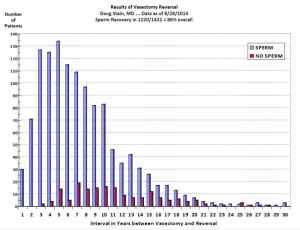
The guidelines set forth by the American Society for Reproductive Medicine and the Society for Male Reproduction and Urology emphasize that overall postoperative conception rates after vasectomy reversal are relatively high, ranging from 50% to 70%. Moreover, the presence of anti-sperm antibodies does not consistently correlate with postoperative fecundability, making the value of preoperative anti-sperm antibody testing a matter of controversy.
Here’s a summary of the research evidence on this subject:
Note: One Stop Medical Center provides the service of Vasectomy Reversal. We have two office locations in Edina, Minnesota, and Casselberry, Florida. If you are interested in vasectomy Reversal, Please fill out the online registration first, we will call you in 2 business days, or please call us at 1-888-992-0019 if any questions.






 From self-order kiosks to robot vacuum cleaners and robot cafes, the rise of robot-assisted experiences in recent years has been undeniable. But would you ever consider participating in a robot-assisted surgical procedure?
From self-order kiosks to robot vacuum cleaners and robot cafes, the rise of robot-assisted experiences in recent years has been undeniable. But would you ever consider participating in a robot-assisted surgical procedure? However, costs aside, it’s still noteworthy to highlight the reliability and effectiveness of robot-assisted vasectomy reversals.
However, costs aside, it’s still noteworthy to highlight the reliability and effectiveness of robot-assisted vasectomy reversals.  Do inform your doctor about any other medications you may be taking.
Do inform your doctor about any other medications you may be taking. Myth: In Vitro Fertilization (IVF) is quicker and easier than having a vasectomy reversal.
Myth: In Vitro Fertilization (IVF) is quicker and easier than having a vasectomy reversal. Myth: Couples should not try to conceive right after a vasectomy reversal for fear of a “leftover, defective sperm.”
Myth: Couples should not try to conceive right after a vasectomy reversal for fear of a “leftover, defective sperm.”